Imagine a world where a simple infection such as strep throat, which affects more than 600 million people annually, is deadly. This was the case until the late 1920s when the invention of penicillin sparked the widespread use of antibiotics. This discovery is often thought of as one of the greatest advances in civilization. However, a problem is threatening its title: antibiotic resistance.
“Resistance happens when germs like bacteria and fungi develop the ability to defeat the drugs designed to kill them,” according to the Centers for Disease Control and Protection. This means that the bacteria do not respond to the antibiotics and continue to grow, becoming difficult to treat and possibly deadly. This is also known as antimicrobial resistance or AMR. In 2019, AMR was directly responsible for the deaths of 1.27 million and associated with the deaths of 4.59 million worldwide. We are facing a future where once easily treatable infections can become life-threatening, and although the consequences of inaction are too severe to ignore, society’s relationship with antibiotics poses a challenge.
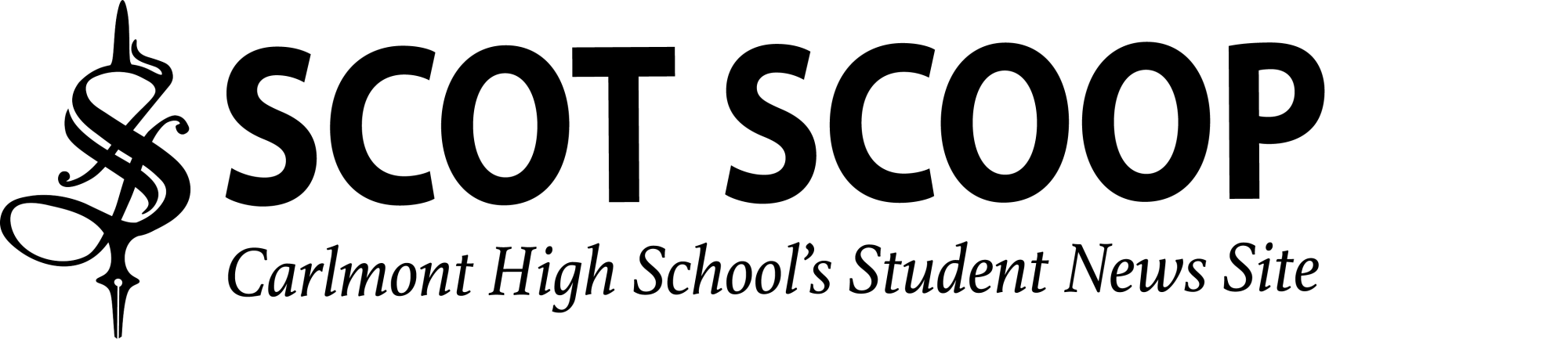
There’s a widespread misunderstanding about antibiotics, ranging from doctor overprescription to consumer misuse. In 2015, a World Health Organization multi-country survey reported that “Close to one-third (32%) of people surveyed believe they should stop taking antibiotics when they feel better, rather than completing the prescribed course of treatment.” 64% of respondents believe antibiotics can be used to treat colds and the flu, despite the fact that antibiotics have no impact on viruses. This is not all. In many undeveloped countries, antibiotics are unregulated and available without a prescription. In this absence of regulation, antibiotics are widely available and inexpensive, encouraging overuse, and subsequent resistance. Even in the U.S., a 2016 study found that doctors substantially overprescribed antibiotics for 3 common conditions that account for 34 million antibiotic prescriptions annually.
So why aren’t scientists creating new and better antibiotics to treat infections? The antibacterial market is broken. With complex science and the research and development process being expensive, time-consuming, and prone to failure, no new classes of antibiotics have been discovered since the 1980s. Think about it this way: medical practitioners cannot use antibiotics to treat chronic issues. This means that big pharmacies make less profits researching new science around antibiotics than medications for chronic conditions. Subsequently many pharmaceutical companies prefer to invest in chronic medical treatment. But this should not be acceptable, and policymakers should be doing more to encourage investment. While some efforts, such as the CDC’s Antibiotic Resistance Solutions have been implemented, there still remains an uphill battle. In 2017, the only state in America having passed a bill to monitor and track antibiotic-resistant infections and deaths was California.
Antibiotic resistance is not only dangerous to one’s health, but also to the economy and to the well-being of society. When they can no longer treat infections, first-line antibiotics must be replaced with more expensive medications. This leads to longer hospital and treatment stays, resulting in higher healthcare expenses and a greater financial strain on families. It is crucial to work together to spread awareness, enact new regulations, and mobilize research efforts. Failure to act now will have catastrophic effects on the future of public health.