“It’s murder.”
“They’re just giving up.”
“Doctors are helping them commit suicide.”
Euthanasia, the practice of ending a patient’s life to limit their suffering, is a widely debated ethical issue. From individual comments on euthanasia to the many varying laws surrounding the practice, differing opinions on the issue are evident.
In the medical ethicists’ world, there are many different terms for euthanasia, each with its own meaning. Generally, the term “active euthanasia” encompasses many different subsets of euthanasia as it refers to the action of a physician prescribing and/or administering a fatal dose of medication to a patient.
Assisted euthanasia occurs when the patient administers the means of death but with the help of another person. “Mercy-killing,” though not an official medical term, is when someone kills a patient without their verbalized consent with the intention of ending their suffering. Finally, the phrase “physician-assisted suicide” typically refers to when the physician gives the patient the means to kill themself, but the patient is the one who carries through with it.
Currently, active euthanasia is legal in Australia, Belgium, Canada, Colombia, Luxembourg, the Netherlands, New Zealand, and Spain. In the United States, although euthanasia is illegal, Medical Aid in Dying (MAID) is legal in California, Colorado, Hawaii, Maine, New Jersey, New Mexico, Oregon, Vermont, Washington, and Washington, D.C.
MAID is outlined as when a physician provides a competent adult who has a terminal diagnosis with a prescription for a lethal dose of a drug at the request of the patient. In California, the End of Life Option Act (ELOA) is the MAID law.
Most people request MAID when they lose autonomy, lose the ability to participate in activities that give their life meaning, or lose dignity because of their illness. However, many people disapprove of the decision to request MAID.
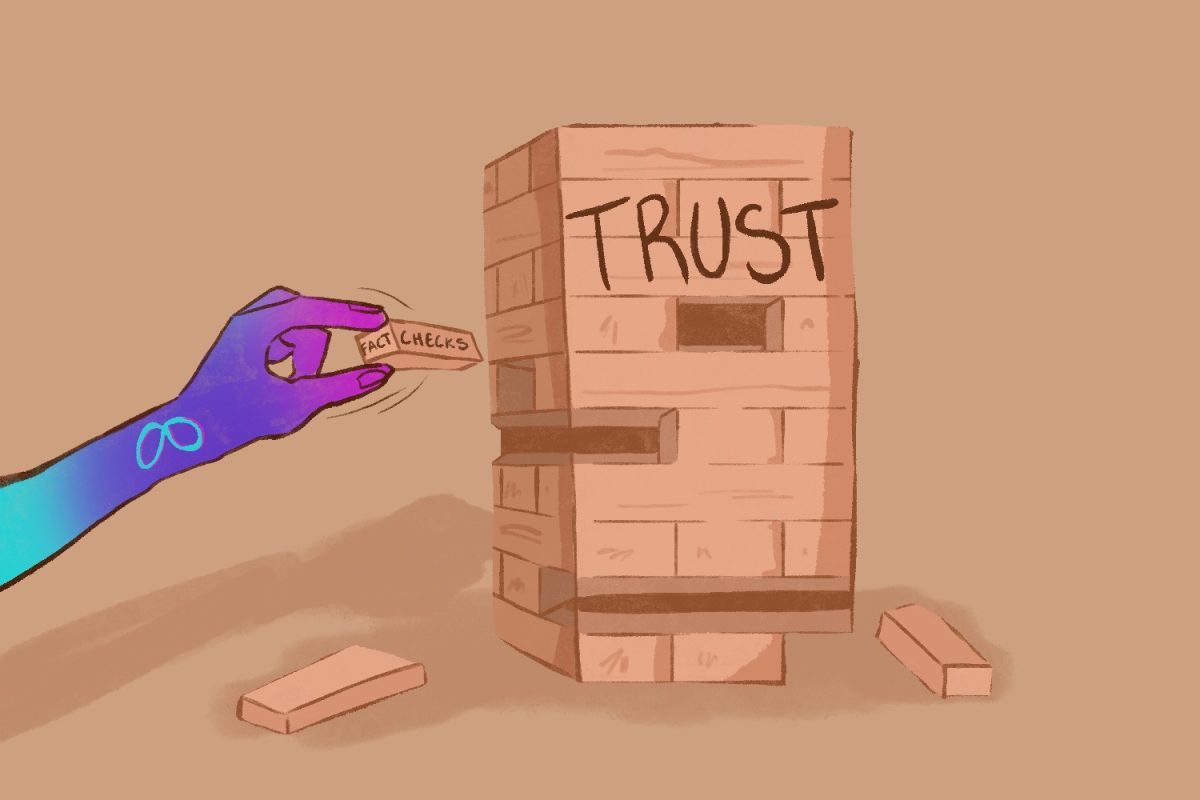
For example, MAID and euthanasia are often viewed as murder, even if the intention is to ease the pain of the patient. Some also argue that MAID and euthanasia are no longer necessary with the development of palliative care — this kind of care is specialized for people living with a severe illness and is designed to help relieve their symptoms and cure their disease.
However, neither argument gives proper consideration to the patient’s quality of life. If a patient is diagnosed with a terminal illness that elicits pain and hinders them from doing activities they enjoy, they do not have a good quality of life.
With ELOA, a patient must have six months or less left to live in order to request the medication to end their life. After receiving the medication, the patient has the right to choose when to take it, or they can decide not to take it at all. This gives them the freedom to decide when and how they want to die, which can be comforting for those who have had their freedom to choose stripped away by their disease.
Meanwhile, some will argue that MAID and euthanasia weaken respect for the sanctity of life or that it may not be in the patient’s best interests. They argue that every human life has its own value and that there’s always a chance the patient can recover, so they should not give up.
While it is true that misdiagnoses are possible, ultimately, the decision as to whether or not to choose MAID or euthanasia is the patient’s. Showing adequate respect for people who are autonomous, meaning they are competent enough to make their own informed decisions regarding their medical care, means giving them the right to decide how they want to live their lives. This includes the right to choose MAID.
Everyone deserves a choice, whether they decide to continue fighting or decide to end their pain and rest. Patients who choose MAID, euthanasia, ELOA, or anything of the like are not giving up, committing suicide, or being murdered by their doctor.
They are choosing to die with dignity.
*This editorial reflects the views of the Scot Scoop Editorial Board and was written by Arianna Zhu.
The Editorial Staff staff voted 9 in agreement, 3 somewhat in agreement, and 4 refrained from voting.