In October 2023, California Gov. Gavin Newsom vetoed the insulin price cap bill, Senate Bill 90, which would have limited insurance and pharmaceutical companies to have patients pay $35 at most for a 30 day supply of insulin vials.
However, Newsom’s veto was extremely detrimental, as the delay in action prevents patients from immediate relief of their financial burden and exacerbates their health condition.
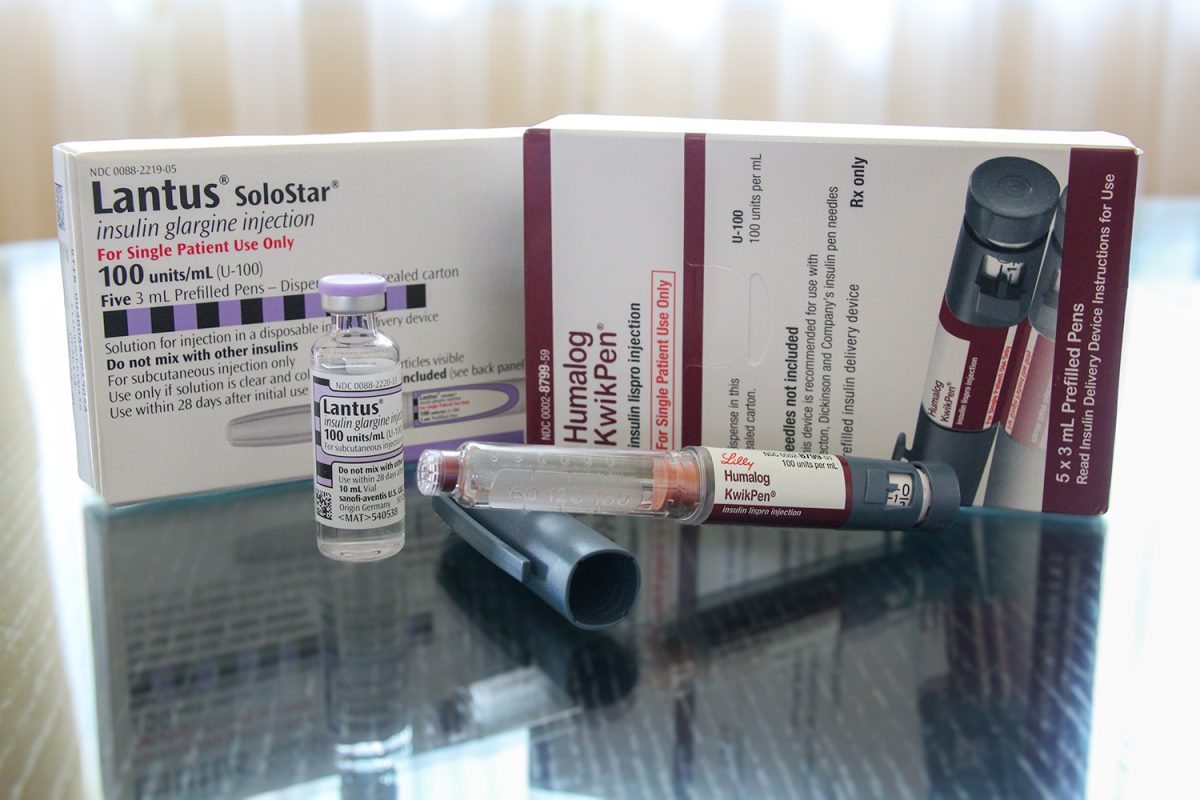
Insulin is vital for patients with diabetes, especially Type 1 diabetes, to regulate their blood glucose levels and survive. Since their body cannot produce insulin alone, they rely on daily injections to manage blood glucose levels.
As of 2021, one in 10 adults in California have been diagnosed with diabetes, and another 272,814 cases are diagnosed each year. The prevalence of diabetes highlights the need for affordable insulin, especially considering the financial strain it inflicts on patients.
According to the American Diabetes Association, spending on insulin tripled from $8 billion in 2012 to $22.3 billion in 2022, a hefty seven to 10 times more than other countries pay.
As a result, patients, particularly those with low incomes, are left to choose between buying food or medication, or, contrarily, have limited amounts of both.
According to an article published by the National Library of Medicine, one in four patients report that they cannot afford insulin. Inevitably, they ration their insulin doses either by skipping doses, using less insulin than prescribed, or delaying the purchase of insulin.
This poses even more severe health complications, such as heart disease, stroke, and death. To prevent more deaths, the government needs to take immediate action to lower the cost of insulin – something that SB 90 does — and Newsom’s plan does not.
While Newsom stated that California has its own partnership with Civica Rx to manufacture and sell insulin for at most$30, this is not a suitable substitute because of the ambiguous timeline.
Since he announced this plan following his veto of SB 90, insulin production has not started. In fact, there is no timeframe for U.S. Food and Drug Administration (FDA) approval.
Newsom also said that creating California’s own insulin targets the underlying high cost of pharmaceuticals, while price caps increase insurance premiums.
However, according to an analysis of the bill by the California Health Benefits Review Program (CHBRP), insurance premiums would only increase by 0.02%. The average cost of insulin per prescription would decrease from $61 to $20.
Meanwhile, Newsom’s plan requires a facility to manufacture insulin, clinical studies to get FDA approval, and sufficient funding to sustain the program. These costs all add up.
In California’s supposed movement toward affordable insulin, the people who would be most impacted are rather left behind to continue grappling with the stress of buying expensive medication.
SB 90 would have provided patients with fast-acting and straightforward relief from this burden, as it would have capped any vial of prescribed insulin at $35.
Even if Newsom wanted to continue with his initiative, SB 90 would be an effective placeholder so patients could have access to affordable insulin throughout the development and eventual approval of Newsom’s plan.
Federal and state governments have already enacted insulin price caps to provide relief for patients. Locally, Santa Clara County began a $1 million grant program for insulin users, according to CalMatters.
With local options to provide quick assistance to patients already in effect, it is imperative that California follow suit.