“She’s not my sister.”
That’s the last thing anyone wants to hear their sibling say, but that’s where Callie Kenady found herself, standing beside her sister who suffers from Alzheimer’s disease.
Confusion, mood swings, and memory loss are all symptoms of the neurodegenerative disease. A disease of the brain, Alzheimer’s causes nerve cells, or neurons, to slowly degenerate and die. This leads to a loss of cognitive function and memory, according to a publication by Roche.
There is no cure.
Kenady, like so many others, knows how painful it is to have a loved one diagnosed with Alzheimer’s and to watch them lose a part of who they used to be.
“I mean, we were oil and water, but we complemented each other so well,” Kenady said.
The Kenady sisters were born and raised in San Francisco where they campaigned together for women’s rights and equal job opportunities. They both wound up in Los Angeles where Callie’s sister Melissa fell in love with a career as a wholesale representative shoe seller. Eventually, the Kenadys would reunite in San Francisco, sharing an apartment flat together.
Both sisters were busy for many years working, traveling, and otherwise living their lives as any person does. They were completely stunned when in 2017 Melissa was diagnosed with Alzheimer’s at the age of 66, though in hindsight Callie said there were some signs. Alzheimer’s diagnosis before the age of 65 is considered early onset, according to the National Institute on Aging, and is a devastating diagnosis.
“I thought, ‘How could this be? People who are our parents’ age are the ones with Alzheimer’s,’” Callie said. “The doctor told us the median life expectancy for someone after you’re diagnosed is around 10 years, so you’re just staring at a fixed calendar. It’s frightening.”
At first, Melissa’s symptoms were mild, such as forgetting where she parked her car, accidentally ordering food twice, and struggling to manage her own finances properly. But as the disease progressed, so did her symptoms.
Melissa developed aphasia, a loss of speech comprehension and the ability to form clear phrases out of words, which is commonly caused by the neurodegeneration seen in Alzheimer’s, according to a paper published by Sage Journal.
“Melissa had always been really articulate, really good at vocabulary, and really good at pop culture. She had a People’s Magazine subscription and lots of other subscriptions she loved to read,” Callie said.
But Melissa eventually lost more and more of her speech. She still enjoys being around people and tries to engage in conversations through her body language and facial expressions, but she’s unable to find the words she once used so robustly.
Despite Melissa’s efforts to remain engaged and fight against her Alzheimer’s, it takes a huge toll on her both mentally and physically. Callie explained how partaking in a seemingly simple task, such as a conversation with family, is incredibly taxing and exhausting for Melissa. Her brain just doesn’t have the same level of function.
Melissa grew frustrated at her sister for trying to help, angry with herself for her lack of independence, and deeply upset and depressed by the effects and consequences of her diagnosis.
“She wouldn’t put herself out there because she didn’t want to look inadequate,” Callie said. “It’s like if you’ve ever been in a situation where you’re playing a game and everybody else is playing much better than you and you know they’re going to make you feel bad about it.”
But as much as Melissa struggled, Callie was right there beside her sister, helping her and fighting for her. They attended therapy sessions together, went to support groups, planned outings, and cared for each other.
Above all, what Melissa needed was her sister.
“She wanted me to be her sister, not her manager,” Callie said.
So that’s what Callie did.
For a while Melissa had caretakers helping her at home so Callie could continue to just be the supportive sister Melissa needed, but when the pandemic hit and everyone began to quarantine Callie realized some changes needed to be made.
“COVID was a mixed blessing. It didn’t demand a lot of me, but Melissa wasn’t getting any kind of engagement with people outside of me, my then-boyfriend, and her caregivers. It was tough.” Callie said. “But she went into a senior community around January 2021.”
Melissa has lived at several different senior communities since then but recently settled into a memory assisted living residence in Berkeley, just a half-hour’s drive away from her sister. Living in memory care provides Melissa with the support and stimulation she needs to live her life to the fullest despite her Alzheimer’s.
Receiving 24/7 support has been helpful for both Kenady sisters, and Callie is aware of how fortunate she is to have such resources.
“The monthly is $10,000 for Melissa’s assisted living, but I was talking to a fiduciary who manages the money of a man with memory loss and 24/7 care,” Callie said. “It’s $30,000 a month.”
Money is commonly one of the biggest issues surrounding Alzheimer’s care, not just in terms of costs for family members, but also in home caretakers, care facilities, employees, and more.
Annual medical and care costs for Medicare beneficiaries with Alzheimer’s are $41,757.
In 2022, the total cost of Alzheimer’s and dementia care is expected to reach $321 billion according to the Alzheimer’s Association, and that number is only going to increase as the world population continues to age.
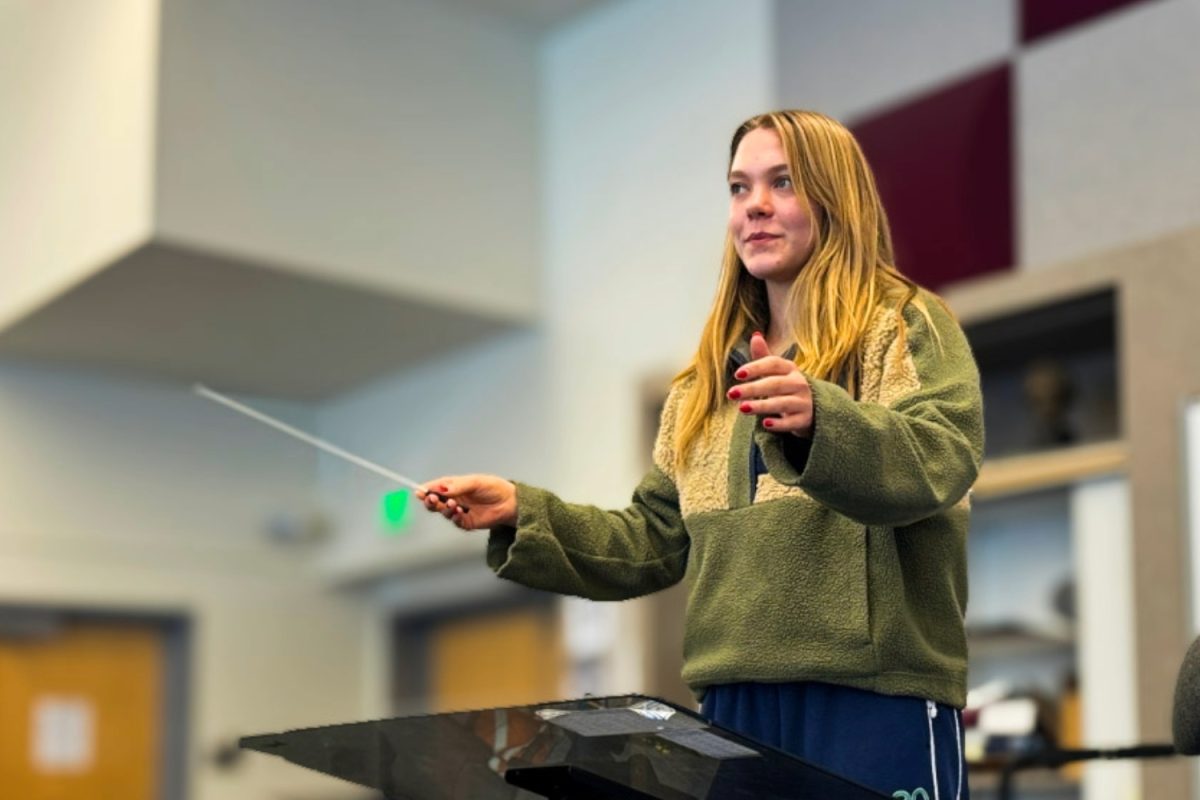
“We’re going to have a tremendous elder population as the baby boomers get older, and we’re going to really need to take care of the people who take care of the elders,” said Miriam Weisberg, the memory services director at Elegance Berkeley.
And it’s true. There are currently over 6 million people with Alzheimer’s in America alone, and that number is projected to reach as high as 16 million by 2050, according to a publication by BrightFocus Foundation.
But regardless of the number of Alzheimer’s patients that will be needing care in the years to come, everyone gets old. Everyone will need help eventually. Weisberg explained that Alzheimer’s is a disability, and as a disability advocate she strives to find the resources to support disabled people in an able-bodied world.
“We’re always going to have people that are different in our society, and it’s a part of the human experience to go through pain and suffering,” Weisberg said. “I would like to see less obsession with curing and more obsession with creating an equal society that has room for people that are different.”
Some of the people making the most impactful differences in the lives of Alzheimer’s patients are the caretakers and directors like Weisberg who spend their days helping and supporting residents in assisted living, and that’s where the money and support should be going.
“We’re not getting paid like computer programmers, even though we’re doing the most important work,” Weisberg said.
But there’s not enough help. Working with the elderly is not a glamorous job, and it doesn’t pay well enough to create more appeal, explained Weisberg. She has a Master’s Degree and spends her days changing diapers and endlessly adjusting the volume of the television.
It takes a certain kind of person to be able to handle the emotional and physical challenges of working with Alzheimer’s patients every day, Weisberg said, but she knows that this is her calling.
“It’s very, very difficult. Extraordinarily difficult,” Weisberg said. “You put your residents before everything.”
But to Weisberg it’s worth it, and her residents and their families certainly agree. While Alzheimer’s is a devastating disease, so many people out there still strive to live their lives to the fullest, despite the difficulties.
Fortunately, there is some hope on the horizon for Alzheimer’s patients in terms of medical treatments. While there is still no cure for Alzheimer’s, a recent study on the drug Lecanemab shows promising advancements in drug discovery.
Alzheimer’s research focuses on certain pathologies in the brain, or abnormalities caused by the disease, explained Jasi Atwal, a senior scientist at Genentech. The two main pathological features of Alzheimer’s are proteins called Tau and Amyloid Beta that aggregate, or clump together and cause issues.
“The main idea behind Alzheimer’s research right now is that we could target those aggregates and that would maybe help people suffering from the disease,” Atwal said.
Alzheimer’s research is historically difficult, namely because it’s a disease of the brain and is much less accessible, Atwal explained.
But the recent clinical trial on the Lecanemab drug may be helping to turn the tide in favor of research targeting Amyloid Beta.
“In clinical trial, there are several phases, and phase three is the definitive study in a large population where you try to show statistical significance,” Atwal said. “In this trial, they were able to do that, and showed that when patients were taking the drug, it slowed the progression of the disease.”
While this is far from a cure for Alzheimer’s, it’s a huge step in the right direction. Atwal shares her excitement with the rest of the scientific community as Alzheimer’s research progresses.
Alzheimer’s is a very real and pressing issue, as more than 10% of all Americans over the age of 65 have Alzheimer’s, according to the Alzheimer’s Association. There is a very real chance that anyone could be facing this disease, including family members and loved ones.
Callie and Melissa fight every day to treasure the moments they have together. No matter how much their lives have changed, they are still sisters.
Like so many others facing Alzheimer’s around the world, life goes on.
“Life isn’t over,” Weisberg said. “It’s just different. And we’re going to adapt and we’re going to change. We’re just going to have a different experience of life.”